synchronisation
of corpuls3 and corpuls cpr
Teamwork to perfection
We have had this vision for a long time: The perfect interaction between corpuls3 and corpuls cpr during resuscitation. Raising the resuscitation processes to the next level of quality was our goal. With its revolutionary modular design, the corpuls3 stands out from other compact devices. It can be separated into the Monitoring Unit, Patient Box and Defibrillator/Pacer. Thanks to the synchronized therapy, stress amongst the team can be significantly reduced. corpuls3 and corpuls cpr become one and when integrated into the team, this duo makes resuscitation even more efficient. Hands-off time is significantly reduced* and the patient's chance of survival is increased – even under the most difficult conditions where space is at a premium.
* Refer to the chapter "Abstract Study"

Full control – at any time
During synchronized therapy, the corpuls3 is not just the remote control for the corpuls cpr – although that is also possible. The corpuls cpr has been perfectly integrated into the AED and manual mode of the corpuls3. Therefore giving the rescue team the ability to treat the patient in accordance with the current guideline recommendations. The corpuls3 shows all the required information on its display.
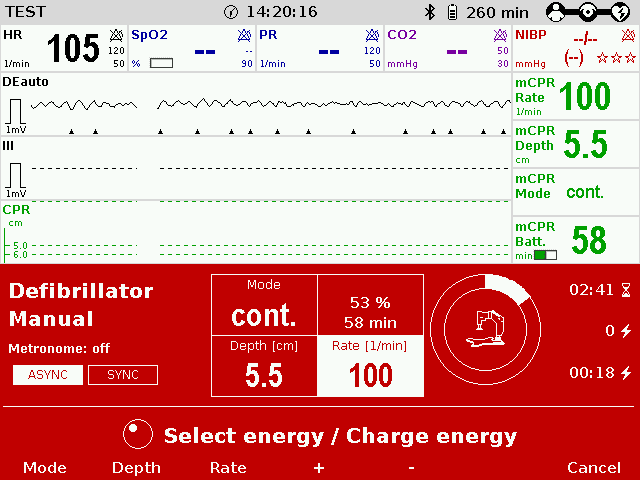
Intelligent control with the corpuls3
The intelligent control of the corpuls cpr by the corpuls3 during a resuscitation follows the current guideline recommendations – depending on the mode (AED, Manual-ERC, Manual-AHA). In each of the modes, the entire rhythm analysis is controlled via the corpuls3 as the central operating unit. The user only needs to monitor the correct position of the stamp on the corpuls cpr. All control commands for the user take place wirelessly between corpuls3 and corpuls cpr.
Starting situation:
The corpuls cpr is positioned on the patient and is performing chest compressions. There is a Bluetooth connection to a corpuls3.
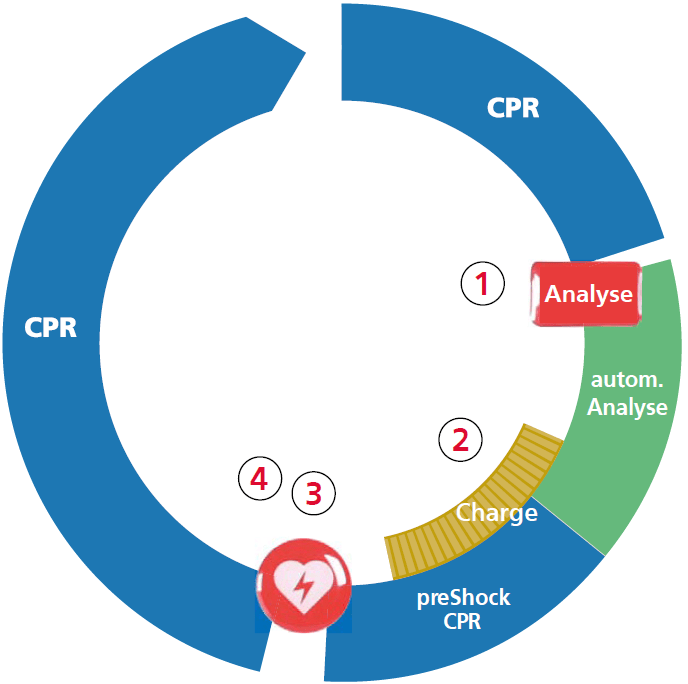
aed-mODE
- Analyse key interrupts the corpuls cpr for the AED analysis and then automatically continues the therapy by corpuls cpr.
- If the rhythm is shockable, the defibrillator is charged and automatic preShock CPR is performed.
- The Shock key interrupts the corpuls cpr for shock delivery.
- If the rhythm is not shockable, the corpuls cpr therapy is automatically continued.
MANUAL 1 (procedure according to erc)
- The stop mCPR key on the corpuls3 interrupts the corpuls cpr for manual rhythm control.
- The Start mCPR key resumes chest compressions/preS hock CPR.
- If the rhythm is shockable, the Shock key interrupts the corpuls cpr for shock delivery.
- If the rhythm is not shockable, the Start mCPR key continues the therapy by the corpuls cpr.

MANUAL 2 (procedure according to AHA)
- Charge key loads the defibrillator.
- The Stop mCPR key on corpuls3 interrupts the corpuls cpr for manual rhythm control.
- If the rhythm is shockable, the Shock key interrupts the corpuls cpr for shock delivery.
- Start mCPR key resumes the therapy by the corpuls cpr.

Application
Whether in a stairwell, on an aerial ladder or in alpine terrain, access to operate the corpuls cpr is often restricted.
With the synchronized therapy, the stretcher being out of reach is no longer a problem. The user always has an overview of all values and can react immediately.

In air rescue, patient access is extremely limited, and rescuers are belted into their seats. Thanks to the perfect interaction of the corpuls3 with the corpuls cpr, movement within the cabin can be reduced. The emergency physician can now treat the patient with mechanical chest compression alone, without having to accept long hands-off times.

Urgent transport always carries high risk for the patient and the rescue team – especially if the team must work while standing. Thanks to the synchronized therapy, the emergency team can remain buckled up while driving. Rhythm control and shock delivery can be performed on the corpuls3 while the rescuer is seated.


In the event of a possible radiation exposure, the corpuls cpr can remain on site and be controlled by the corpuls3 from a safe distance. The corpuls cpr radiolucent boards and the fact that the corpuls3 can be divided into its three modules, make both devices ideal partners in the cardiac Cath Lab, for example. With the synchronized therapy, there is no need to intervene in the sterile operating room.

Abstract Study
The ERC guidelines recommend the shortest possible compression interruptions during cardiopulmonary resuscitation. Before and after the shock delivery, chest compressions should be interrupted for a maximum of 10 seconds. A peri-shock pause (the compression break before and after defibrillation) of a maximum of 10 seconds has been scientifically proven to be associated with a higher survival rate (Cheskes et al. 2014; Sell et al. 2010). According to the ERC guidelines, the entire manual defibrillation process should be possible with a compres-sion break of less than 5 seconds (Monsieurs et al. 2015). When using the corpuls3 in combination with the corpuls cpr in an in-house study, these recommendations could be noticeably undercut. With the synchronisation of the corpuls3 and the corpuls cpr, this endeavour could be further increased. With synchronized device operation, the hands-off time was reduced by 16.08%.

Representation of the hands-off time of our study comparing synchronized and disconnected device operation of the corpuls3 and corpuls cpr.
(Significance P < 0.001: ***; P < 0.05: *)
The reduction in the compression pause is particularly evident during the perishock pause. On average, the perishock pause in synchronized mode of 2.00 ± 0.32 s is 38.23% shorter than the peri-shock pause in disconnected mode of 3.24 ± 0.71 s. This saving can be a valuable gain in time with the desired break being a maximum of 5 seconds.

When comparing the peri-shock pauses, the significant minimization of the pause duration with synchronisation compared to disconnected device operation of corpuls3 and corpuls cpr becomes particularly clear.(Significance P < 0.001: ***)
References
Cheskes, Sheldon; Schmicker, Robert H.; Verbeek, P. Richard; Salcido, David D.; Brown, Siobhan P.; Brooks, Steven et al. (2014): The impact of peri-shock pause on survival from out-of-hospital shockable cardiac arrest during the Resuscitation Outcomes Consortium PRIMED trial. In: Resuscitation 85, S. 336–342. DOI: 10.1016/j.resuscitation.2013.10.014.
Kleinman, Monica E.; Brennan, Erin E.; Goldberger, Zachary D.; Swor, Robert A.; Terry, Mark; Bobrow, Bentley J. et al. (2015): Part 5. Adult Basic Life Support and Cardiopulmonary Resuscitation Quality. Circulation. 2015;132[suppl 2]:S414–S435. In: Circulation 132 (18 suppl 2), S. S414-S435. DOI: 10.1161/CIR.0000000000000259.
Monsieurs, Koenraad G.; Nolan, Jerry P.; Bossaert, Leo L.; Greif, Robert; Maconochie, Ian K.; Nikolaou, Nikolaos I. et al. (2015): European Resuscitation Council Guidelines for Resuscitation 2015: Section 1. Executive summary. Resuscitation 95 (2015) 1–80. In: Resuscitation 95, S. 1–80. DOI: 10.1016/j.resuscitation.2015.07.038.
Nolan, Jerry P.; Soar, Jasmeet; Zideman, David A.; Biarent, Dominique; Bossaert, Leo L.; Deakin, Charles D. et al. (2010): European Resuscitation Council Guidelines for Resuscitation 2010. Section 1. Executive Summary. In: Resuscitation 81 (10), S. 1219–1276. DOI: 10.1016/j.resuscitation.2010.08.021.
Perkins, Gavin D.; Olasveengen, Theresa M.; Maconochie, Ian; Soar, Jasmeet; Wyllie, Jonathan; Lockey, Robert Greif Andrew et al. (2017): ERC 2017 Guidelines Update. In: Resuscitation. DOI: 10.1016/j. resuscitation.2017.12.007.
Sell, Rebecca E.; Sarno, Renee; Lawrence, Brenna; Castillo, Edward M.; Fisher, Roger; Brainard, Criss et al. (2010): Minimizing pre- and post-defibrillation pauses increases the likelihood of return of spontaneous circulation (ROSC). In: Resuscitation 81 (7), S. 822–825. DOI: 10.1016/j.resuscitation.2010.03.013.
corpuls simulation – train before you fight
There is often a big difference between theoretical scenarios and actual missions. With corpuls simulation we bring completely realistic scenarios to your training. Just as pilots training in a flight simulator are thrown surprise complications, rescuers training with corpuls simulation have to overcome unforeseen situations. The result is a team that is optimally prepared for every scenario and therefore, a significantly better quality of care for the patient.

Training not only means using existing knowledge, but also learning new techniques – that includes synchronized therapy with corpuls3 and corpuls cpr. Thanks to the Bluetooth connection from corpuls simulation, this feature can now be trained realistically at any time. All usage scenarios and benefits can be optimally taught for use in the field: simply connect corpuls simulation with the corpuls cpr (from software version 1.2) and take your training to a whole new level.
* Using the combination of corpuls simulation and corpuls cpr only on training manikins





